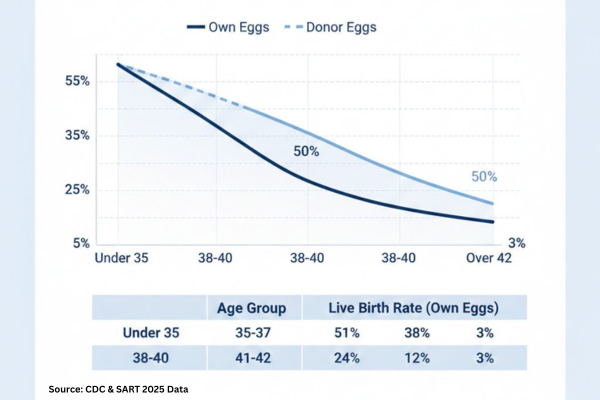
Embryo Transfer Timing and Protocols for Higher Pregnancy Rates focus on aligning embryo development, uterine receptivity, and individualized clinical decisions to improve the chances of implantation and live birth in IVF treatment. For many people, embryo transfer feels like the moment where hope and science finally meet. In 2023, the average IVF pregnancy rate per embryo transferred in fresh cycles was about 31%, with women aged 18–34 reaching roughly 41% per embryo, so how and when we plan embryo transfer can make a real difference to how close you get to a positive result.
Key Takeaways
| Question | Short Answer |
|---|---|
| What is embryo transfer timing in IVF? | It is the decision of which day (for example, day 3 or day 5) and which cycle conditions to transfer embryos into the uterus, typically as part of our IVF procedures and treatment plan. |
| Is day‑3 or day‑5 transfer better? | Studies suggest overall live birth chances can be similar, so we individualize the choice; some data show short‑term advantages for blastocyst (day‑5) transfer in selected patients. |
| How do hormones affect transfer success? | Double embryo transfer may raise per‑transfer pregnancy odds but also increases twin risk, which we explore in our article on double embryo transfer and the likelihood of twins. |
| Does age change the best protocol? | Yes, embryo transfer strategy often differs by age, as explained in our overview of IVF success rate by age. |
| Should we transfer one or two embryos? | Double embryo transfer may raise per‑transfer pregnancy odds but also increases twin risk, which we explore in our article on double embryo transfer and likelihood of twins. |
| Can frozen embryos work as well as fresh? | Modern data show both fresh and frozen transfer strategies can give meaningful outcomes, especially when supported by thoughtful cryopreservation and embryo freezing protocols. |
| What else affects embryo transfer success? | Factors like embryo quality, age, uterus health, and lab techniques all matter, which we summarize in our guide to factors affecting IVF success. |
1. Understanding Embryo Transfer Timing In The IVF Journey
Embryo transfer is the point in an IVF cycle when we place one or more embryos into the uterus, aiming to match embryo development with the uterus at its most receptive stage.
Timing covers several layers, including which day the embryo is transferred, whether it is a fresh or frozen transfer, and what is happening hormonally in your body that day.
How Embryo Transfer Fits Into The IVF Process
In a typical IVF pathway, we start with ovarian stimulation, then egg retrieval, fertilization in the lab, and culture until the planned transfer day.
Our overview of IVF procedures and treatments explains these steps and how embryo transfer is coordinated with monitoring, medication, and follow‑up.


What “Higher Pregnancy Rates” Really Means
When we talk about higher pregnancy rates, we are usually referring to clinical pregnancy or live birth per transfer or per complete IVF cycle, not just positive tests.
Different studies use different definitions, so we always interpret data with care and emphasize that no protocol can guarantee a specific outcome for any individual.
The Role Of Individualization
Research shows that what works best statistically across large groups is not always the best choice for every single patient.
That is why we look at age, medical history, embryo number and quality, and practical issues like work schedules before recommending a transfer plan.
2. Day‑3 vs Day‑5 Embryo Transfer: What Research Suggests
One of the most common questions we hear is whether a day‑3 (cleavage stage) or day‑5 (blastocyst) transfer is “better.”
Current evidence suggests that, when you look at cumulative live birth across a full treatment horizon, both strategies can perform similarly for many good‑prognosis patients.
Comparing Day‑3 And Day‑5 Outcomes
A large 2024 randomized trial found no meaningful difference in cumulative live birth rates between blastocyst transfers and cleavage‑stage transfers in good‑prognosis groups, with figures reported around the high‑50% range in each arm.
In the same line of research, some analyses report higher short‑term cumulative live birth percentages after blastocyst transfer within a year, which suggests that for certain patients, day‑5 transfer may front‑load chances of success.
Why Some Clinics Prefer Blastocysts
Blastocyst culture allows more time to observe embryo development, so we can often select embryos that appear more likely to implant based on standardized lab criteria.
This can be helpful when you have several good‑quality embryos, since embryo selection becomes a key part of the protocol.
Why Day‑3 Can Still Be A Sensible Choice
For patients with fewer embryos, or when embryos seem delicate in culture, transferring on day 3 can reduce the time embryos spend in the lab environment.
Some centers also choose day‑3 transfer if laboratory capacity or patient‑specific clinical considerations make extended culture less suitable.

Balancing Evidence And Personal Factors
When we plan timing, we combine the best available research with your own history, embryo information, and comfort with different strategies.
Because studies use specific inclusion criteria, their results might not fully reflect the experiences of patients with more complex fertility backgrounds.
3. Fresh vs Frozen Embryo Transfer: Timing Across Cycles
Another major timing decision is whether to transfer embryos fresh in the same cycle as egg retrieval, or freeze them for transfer in a later cycle.
Both approaches are supported by modern evidence, and clinics around the world use each strategy in different patient groups.
How Fresh Transfer Timing Works
In a fresh transfer, we usually schedule embryo transfer 3 to 5 days after egg retrieval in the same stimulated cycle.
The uterus has just been exposed to ovarian stimulation medications, so we monitor lining thickness and hormone levels to judge whether conditions appear suitable.
How Frozen Transfer Timing Works
In a frozen embryo transfer (FET), we cryopreserve embryos and then plan transfer in a later natural or programmed cycle.
This allows time for hormones to return to baseline and for careful planning around uterine receptivity, work, and travel.
What Studies Say About Fresh vs Frozen
Some studies report slightly higher live birth rates after a first fresh transfer compared with a first frozen transfer in particular populations, while others find broadly similar cumulative outcomes when you consider multiple transfers.
These results vary by age, ovarian response, and clinic protocols, so we review data in context and tailor recommendations to each case.

When We Might Suggest Freeze‑All
Some clinics consider a freeze‑all approach in selected situations, for example, when hormone levels at retrieval are very high, the uterine lining is not ideal, or there are specific medical considerations.
This allows us to separate stimulation from implantation attempts, which can simplify both medical monitoring and patient experience in some cases.
A concise visual guide to the five key steps in embryo transfer timing and protocols that can help improve pregnancy outcomes.
Did You Know?
A 2024 multicenter trial found no overall difference in cumulative live birth between day‑5 blastocyst and day‑3 cleavage transfers for good‑prognosis patients, suggesting that timing decisions can often be individualized without losing overall success potential.
4. Hormonal Preparation And Progesterone Timing For Transfer
For embryos to implant, the uterine lining needs to be in sync with embryo development, and progesterone plays a central role in this synchronization.
We focus heavily on the timing and level of progesterone support before and after embryo transfer, especially in frozen cycles and programmed protocols.
Why Progesterone Matters For Implantation
Progesterone helps change the endometrium from a proliferative to a secretory state, which makes it more receptive to an arriving embryo.
Evidence suggests that inadequate or mistimed progesterone exposure can reduce the chances that a good‑quality embryo will attach and continue to develop.
Types Of Endometrial Preparation Protocols
Broadly, we can use natural cycle FET, modified natural cycle, or artificial hormone replacement therapy (HRT) cycles to prepare the uterine lining for transfer.
Randomized trials report that live birth rates between these approaches often fall within a fairly similar range, which supports flexible planning led by patient characteristics rather than one “best” method.
Monitoring Timing In Real Life
In natural or modified cycles, we usually track ovulation by ultrasound and blood tests, then time progesterone start and embryo transfer relative to ovulation.
In artificial cycles, we schedule estrogen and progesterone to mimic a natural pattern, then select a transfer day that matches embryo age, always checking that lining thickness looks appropriate.


Evidence On Natural vs Artificial FET Cycles
Several modern studies report that natural or modified natural cycles can achieve implantation, clinical pregnancy, and ongoing pregnancy rates that are comparable to artificial cycles in many groups.
Some analyses suggest natural cycles may be associated with slightly thicker endometrial linings in selected cohorts, but results differ between centers and patient populations.
5. How Age And Embryo Quality Guide Transfer Protocols
Age influences egg quality, embryo quality, and uterine environment, so it is no surprise that research consistently finds different IVF success rates across age groups.
We use age not as a strict limit, but as a guide to frame realistic expectations and tailor embryo transfer planning.
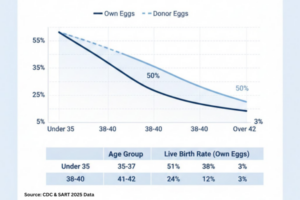
Age‑Related Statistics To Keep In Perspective
Data drawn from international registries show that younger age groups often have higher per‑embryo pregnancy rates, which gradually decline with advancing age.
For example, the 2023 figures mentioned earlier illustrate that women aged 18–34 can see around 41% pregnancy per fresh embryo transferred, while older age brackets typically have lower figures.
Adjusting Protocols For Different Age Groups
In younger patients with several good‑quality embryos, we often focus on single embryo transfer and careful selection, sometimes supported by preimplantation genetic testing where appropriate.
For patients in higher age bands, we may discuss options such as donor eggs or donor embryos if repeated transfers with own eggs are not leading to pregnancy, always respecting personal preferences and values.

The Role Of Embryo Testing And Selection
Preimplantation genetic testing can help identify embryos without certain genetic abnormalities before transfer, which may be especially relevant in cases of known genetic disease risk.
However, PGT does not guarantee success, and results must be interpreted carefully with genetic counseling and detailed discussion of benefits, limitations, and ethical aspects.
6. Single vs Double Embryo Transfer: Balancing Chance And Risk
How many embryos to transfer is a crucial part of any protocol discussion, because it affects both per‑transfer pregnancy chances and the likelihood of twins or higher‑order multiples.
Research indicates that double embryo transfer can raise the chance of pregnancy per transfer but also significantly increases twin pregnancy rates, which carry higher medical risks.
Understanding Single Embryo Transfer (SET)
Single embryo transfer focuses on placing one carefully selected embryo into the uterus, often prioritizing safety and reducing the chance of multiple pregnancy.
For younger patients with high‑quality embryos, SET can offer strong pregnancy potential while limiting many of the obstetric risks linked with twins.
When Double Embryo Transfer (DET) Is Discussed
DET may be considered in some circumstances, such as older age, previous failed transfers, or when embryo quality and number are limited, always with full counseling on twin risk.
Our overview of double embryo transfer and likelihood of twins explains how we weigh these factors and why modern guidelines trend toward SET whenever safe and appropriate.
Multiple Pregnancy And Safety Considerations
Twin pregnancies are associated with higher chances of preterm birth and other complications, so many professional bodies encourage limiting the number of embryos transferred when safe.
We always discuss these considerations clearly so you can make an informed decision that fits your priorities and tolerance for different risks.
Did You Know?
One study on natural‑cycle frozen embryo transfer reported a clinical pregnancy rate of about 59% and ongoing pregnancy around 51%, showing that carefully timed single embryo transfers in FET cycles can achieve substantial outcomes in modern practice.
7. Donor Eggs, Sperm, And Embryos: Timing Considerations In Third‑Party Reproduction
When donor eggs, sperm, or embryos are part of treatment, embryo transfer timing must also accommodate donor cycles, shipping logistics, and additional screening steps.
These factors can influence whether we recommend fresh synchronized cycles, frozen embryo use, or embryo transfers planned well after donor procedures are complete.
Egg Donation Protocols And Transfer Timing
In donor egg cycles, we often synchronize the donor’s stimulation with the recipient’s endometrial preparation, or we freeze embryos created from donor eggs for transfer later.
This flexibility allows us to schedule recipient embryo transfer at a time when uterine conditions look optimal and when the recipient feels ready.
Sperm Donation And Embryo Creation
Donor sperm can be used in both IUI and IVF, and timing is coordinated with ovulation or egg retrieval respectively.
In IVF, once fertilization has occurred, embryo development and transfer timing follow the same principles as in non‑donor cycles, guided by embryo growth and endometrial readiness.
Donor Embryo Adoption And Scheduling
With donor embryo adoption, embryos are usually already frozen, so transfer timing revolves around recipient preparation and administrative steps such as matching and consent.
Once logistics are complete, the medical protocol looks very similar to a standard FET, with attention to lining thickness, hormone levels, and embryo thawing conditions.
8. External Timing Factors: Calendar, Lifestyle, And Environment
Beyond hormones and lab schedules, several everyday factors can subtly influence embryo transfer timing and possibly outcomes.
These include clinic workload, patient availability, and even environmental timing such as daylight saving time changes in some regions.
Daylight Saving Time And Transfer Outcomes
One observational study reported that transfers performed during the week of daylight saving time transition were associated with lower odds of live birth in some patients, especially women over 37.
While this type of research does not prove a direct cause, it raises interesting questions about sleep patterns, circadian rhythm shifts, and how we schedule transfers when possible.
Working Around Life Commitments
We know that work, childcare, travel, and stress levels all affect how patients experience treatment, even if they are harder to measure in statistics.
Whenever possible, we plan transfer timing so that you have realistic space for rest, follow‑up visits, and medication schedules.

Emotional Readiness And Decision‑Making
Evidence‑based medicine is essential, but emotional readiness is just as real when you are deciding whether to proceed with a transfer now or delay.
We encourage open discussion about how you feel so that timing decisions are not based only on lab numbers but also on your capacity to go through the process.
9. Lab Protocols That Support Better Transfer Outcomes
Behind each embryo transfer are many laboratory steps that indirectly affect timing and potential success, such as fertilization technique, culture conditions, and freezing methods.
While patients do not usually see this part of the process, it is central to how we structure transfer protocols and decide when an embryo is ready to go back.
ICSI And Fertilization Timing
Intracytoplasmic sperm injection (ICSI) involves injecting a single sperm directly into an egg, which can be useful in male‑factor infertility or limited sperm scenarios.
ICSI affects the starting point of embryo development timing, so our lab tracks exact fertilization time when scheduling day‑3 or day‑5 transfers.
PGT Biopsy And Transfer Planning
When we perform PGT, we usually biopsy embryos at the blastocyst stage and freeze them while genetic analysis is completed.
Once results are available, we can then schedule a frozen transfer on a day that matches embryo age with endometrial receptivity and patient readiness.
Cryopreservation Techniques And Thaw Timing
Modern vitrification methods allow embryos to be frozen and warmed with high survival rates in experienced labs, which opens more flexibility in transfer timing.
We coordinate thawing with transfer so that the embryo spends the minimum practical time outside controlled lab conditions before being placed into the uterus.
10. Practical Questions To Ask When Planning Your Embryo Transfer
When you prepare for embryo transfer, asking focused questions can help clarify which timing and protocol choices fit you best.
We encourage you to come to consultations with written questions so nothing important is missed in the moment.
Key Questions About Timing And Protocol
Understanding embryo transfer timing and protocols for higher pregnancy rates allows patients to ask more informed questions and participate actively in transfer planning
- Why are you recommending a day‑3 or day‑5 transfer in my case, and what alternatives would look like?
- Will this be a fresh or frozen transfer, and what are the pros and cons of each for me specifically?
- How will my progesterone and endometrial lining be monitored before transfer?
- How many embryos do you suggest transferring, and what does that mean for twin risk?
Questions About Expectations And Follow‑Up
- What are realistic pregnancy and live birth expectations for someone of my age and medical background?
- What happens if this transfer does not lead to pregnancy, and how would that influence timing of the next step?
- Are there lifestyle or scheduling changes you recommend around the transfer date?
Creating A Shared Plan With Your Care Team
Our goal is always to create a shared, transparent plan so you understand why we choose specific timing and protocols rather than feeling that decisions are made behind the scenes.
When you have a clear picture of the rationale, statistics, and alternatives, it becomes easier to move through treatment with confidence and realistic hope.
Conclusion
Embryo transfer timing and protocols bring together science, careful monitoring, and your personal circumstances, and each of these elements can influence the probability of pregnancy.
While research offers useful benchmarks, there is no single universally “best” protocol, so we focus on individualized planning that respects both the data and your unique story, always avoiding medical promises that cannot be guaranteed.
If you are considering IVF or planning an upcoming transfer, we encourage you to explore our educational resources, ask detailed questions, and work with your care team to design a timing strategy that feels medically sound and personally sustainable.
With thoughtful preparation, open communication, and evidence‑informed choices, embryo transfer can be approached as a step that is carefully aligned with both current research and your own goals for building a family.