The pursuit of parenthood is a deeply significant undertaking, frequently complicated for many by the challenges of conception (TTC). Within this complex field, the impact of prolonged psychological and physical strain remains a critical, yet often marginalized, consideration.
Grasping the precise Stress and fertility connection mechanism moves beyond general advice to relax; it involves acknowledging a direct biological pathway that can actively impede reproductive success.
This definitive guide will detail the specific physiological effects of stress on reproductive health, map the self-perpetuating infertility distress cycle, and present eight crucial, evidence-based truths designed to actively optimize your internal environment for fertility.
Understanding the Physiological Stress and Fertility Connection Mechanism
The human physiology is programmed to respond identically to an immediate physical threat and to the sustained, corrosive presence of psychological stress and infertility.
This ancient survival mechanism prioritizes immediate life preservation, immediately suppressing non-essential biological processes—most notably, reproduction. This fundamental physiological re-prioritization forms the bedrock of the Stress and fertility connection mechanism.
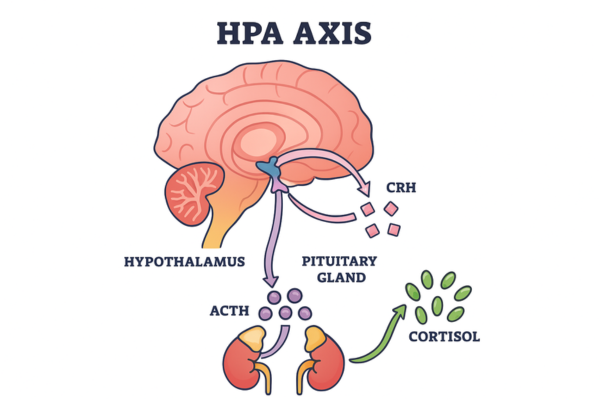
A. The HPA Axis: How the Stress Response Directly Impacts Reproduction
The body’s primary neuroendocrine regulator of stress is the HPA axis (Hypothalamic-Pituitary-Adrenal axis). Perception of threat, whether physical or emotional, triggers the release of corticotropin-releasing hormone (CRH) from the hypothalamus.
This signal cascades to the pituitary and then to the adrenal glands, culminating in a sustained surge of cortisol. While this acute response is protective, chronic elevation directly activates the detrimental Stress and fertility connection mechanism.
The antagonism between cortisol and fertility is profound: sustained high cortisol levels directly inhibit the Gonadotropin-Releasing Hormone (GnRH) pulse generator within the hypothalamus.
GnRH is the essential upstream regulator that commands the pituitary to release the hypothalamic hormones, Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH), which govern ovarian function and egg maturation.
The ensuing effect of this suppression is often stress-induced anovulation or marked menstrual cycle dysregulation. When we observe that stress affects conception, it is frequently through this pathway.
For instance, the reason can stress delay my period? is answered by this hormonal disruption stalls or halts the necessary signals for egg release. Grasping this hypothalamic suppression is paramount to understanding the biological reality of the Stress and fertility connection mechanism.
Moreover, the persistent load of high cortisol compromises the essential estrogen-progesterone balance required for creating and sustaining a receptive uterine lining (endometrium).
Progesterone, a hormone critical for the maintenance of the luteal phase and for facilitating implantation, can be diverted in a process known as ‘pregnenolone steal’ to feed the cortisol production pathway, thereby undermining the conditions necessary for a viable pregnancy.
This detailed hormonal interference underscores the physiological gravity of the Stress and fertility connection mechanism.
B. Cellular Impact: Oxidative Stress and Gamete Health
The Stress and fertility connection mechanism is not limited to systemic hormonal effects; it exerts a damaging influence at the fundamental cellular level by promoting oxidative stress. This state arises from an uncontrolled surplus of reactive oxygen species (ROS) that overwhelms the body’s natural antioxidant capacities.
While low concentrations of ROS are vital for normal cellular function, chronic stress significantly escalates these levels, leading to detrimental damage to cellular components, most critically, DNA. Within the reproductive context, this translates to a potential reduction in female egg quality and a higher rate of DNA fragmentation in sperm.
Both situations directly diminish embryo competence, increasing the probability of failed implantation or early miscarriage. This cellular dimension of the Stress and fertility connection mechanism works subtly but relentlessly, degrading the reproductive material essential for successful conception.
The role of male fertility stress demands equal attention. Persistent psychological pressure can compromise the integrity of the blood-testis barrier, creating an altered microenvironment within the testes. This contributes to suboptimal semen parameters, negatively impacting sperm motility and overall concentration.
Consequently, the Stress and fertility connection mechanism must be viewed as a coupled, dyadic biological challenge. Recognizing and addressing this profound cellular link is essential for any comprehensive strategy to manage reproductive stress.
The Vicious Cycle: Addressing the Stress and Fertility Connection Mechanism in the Context of TTC
For individuals and couples engaged in trying to conceive (TTC), the very intensity of their desire frequently becomes the primary source of emotional pressure, initiating a counterproductive, self-sustaining loop termed the infertility stress cycle. This cycle is a central psychological component of the Stress and fertility connection mechanism.
A. The Infertility Distress and Feedback Loop
The infertility stress cycle functions as a deeply entrenched biological and emotional feedback system. As couples navigate the ongoing struggle to conceive, they experience profound infertility distress—a complex emotional presentation encompassing sadness, isolation, resentment, and a complete loss of control.
This significant emotional burden invariably drives up cortisol levels, which, as established in Section I, powerfully reinforces the physiological Stress and fertility connection mechanism, thereby lowering the probability of conception. Each subsequent cycle failure intensifies the disappointment, tightening the grip of the stress loop.
The lived reality is that the stress of the fertility journey is often perceived as a constant, unrelenting emotional state. Intervening successfully requires focused management of chronic emotional states such as depression and infertility, and the pervasive anxiety and trying to conceive (TTC).
It is entirely appropriate and common for couples to experience intense emotional turbulence due to the recurring monthly rhythm of hope and devastating disappointment. The feeling of failing to achieve a natural human milestone often leads to complex feelings of grief and loss, TTC.
Recognizing and validating this infertility distress is the foundational act required to interrupt the destructive Stress and fertility connection mechanism. Empirical evidence is consistent: a higher measured psychological stress load is demonstrably associated with lower conception probabilities, conclusively proving that stress affects conception.
Importantly, this negative Stress and fertility connection mechanism is exacerbated by fertility treatment itself. The rigid schedules, financial pressure, and physical demands associated with procedures like IVF or IUI significantly amplify the baseline stress response, potentially compromising the optimal environment required for successful outcomes.
Effective intervention, therefore, requires recognizing this psychological feedback loop as a key vulnerability in the Stress and fertility connection mechanism that must be managed through specialized strategies.
B. The Role of Male Fertility Stress
While clinical and social attention frequently centers on the female partner, the Stress and fertility connection mechanism imposes substantial and unique pressures on men.
Male fertility stress commonly presents as profound feelings of inadequacy, pressure regarding performance, and high levels of isolation, largely because men are socially conditioned to be less inclined to engage in support groups or articulate their infertility distress.
As detailed in the cellular analysis, chronic stress, evidenced by elevated cortisol from male fertility stress, can directly undermine the efficiency and output of spermatogenesis, specifically impairing sperm motility and overall viability.
Beyond the physiological, the psychological toll often contributes to situational performance anxiety and potentially erectile dysfunction, factors which strain the partnership and can inadvertently reduce the frequency of timed intercourse during the crucial fertile window.
This combined emotional and biological burden underscores that the Stress and fertility connection mechanism is fundamentally a challenge shared equally by the couple. A truly comprehensive approach requires robustly addressing the male experience.
The understanding that stress affects conception through distinct but interconnected male and female pathways necessitates a holistic strategy for managing the entire pervasive Stress and fertility connection mechanism.
Both partners require access to evidence-based stress reduction techniques and specialized professional support to optimize not only their chances of conception but also their quality of life throughout the fertility journey.
8 Essential Truths for Optimizing the Stress and Fertility Connection Mechanism
Successfully navigating the Stress and fertility connection mechanism requires proactive, consistent effort. These eight essential truths provide a framework for creating an internal environment conducive to conception help.
Truth 1: Implement Mind-Body Practices Daily
To proactively counteract the physiological cascade of the Stress and fertility connection mechanism, consistent daily intervention is non-negotiable.
This involves a dedicated commitment to stress reduction techniques designed to intentionally transition the autonomic nervous system from sympathetic (“fight or flight”) dominance to parasympathetic (rest and digest) regulation.
Effective examples include focused daily mindfulness, diaphragmatic breathing, and structured relaxation exercises. Participation in a formal mind-body program for fertility, which typically integrates cognitive restructuring alongside physical practices such as fertility yoga, demonstrates superior efficacy compared to sporadic efforts.
This intentional, sustained practice is vital for down-regulating the HPA axis and achieving hormonal stability.
Truth 2: Seek Professional and Social Support
The burden of infertility distress is compounded by isolation. It is critical to know when and how to seek a doctor’s advice on stress and conception.
A reproductive endocrinologist diagnoses underlying physical factors, while a mental health professional specializing in reproductive health directly addresses the psychological drivers of the Stress and fertility connection mechanism.
CBT for fertility (Cognitive Behavioral Therapy) is highly recommended, as it provides structured tools to identify and reframe cognitive distortions, thereby cultivating genuine resilience.
Furthermore, engaging with peer support groups offers essential validation and normalizes the complex emotions of grief and loss TTC. This integrated, two-pillar approach—clinical medicine and psychological care—is indispensable for the comprehensive management of the Stress and fertility connection mechanism.
Truth 3: Lifestyle Pillars (Sleep and Nutrition)
The foundational importance of adequate sleep for endocrine health is paramount. Sleep serves as the biological reset period during which the HPA axis naturally de-escalates, facilitating the stabilization of circulating cortisol levels.
Compromised sleep quality acts as both an indicator and a driver of chronic stress, thereby aggressively fueling the negative Stress and fertility connection mechanism.
Clinical discussion often revolves around signs of adrenal fatigue—a functional description of an exhausted stress response system—the management of which must begin with stringent sleep hygiene protocols.
Concurrently, a diet emphasizing whole foods and rich in key antioxidants provides the cellular defense mechanism needed to mitigate the tissue damage caused by oxidative stress, which is a direct consequence of the sustained Stress and fertility connection mechanism.
Truth 4: Monitor Biomarkers
Reliance solely on subjective stress reporting is insufficient. Objective physiological measurement offers essential insight into the true activity of the Stress and fertility connection mechanism.
Key biomarkers include salivary cortisol levels (assessed rhythmically throughout the day) and salivary alpha-amylase, which serves as a highly reliable marker of sympathetic nervous system activation.
Quantifiable data show that elevated alpha-amylase activity correlates with diminished natural conception rates, thereby providing empirical validation and actionable feedback regarding the effectiveness of implemented stress reduction techniques.
Regular monitoring of these objective indicators underscores the necessity and precision required for effectively managing the Stress and fertility connection mechanism.
Truth 5-8: Additional Actions
- Truth 5: Set Boundaries: Strategically limit engagements with individuals or circumstances that generate intense emotional turbulence or unwanted scrutiny regarding the fertility journey. Protect your peace as a priority.
- Truth 6: Consistent, Moderate Movement: Incorporate regular, moderate physical activity (e.g., brisk walking, light cycling). Conversely, be aware that excessive or exhaustive exercise can provoke an additional cortisol spike, which negates the efforts to regulate the Stress and fertility connection mechanism.
- Truth 7: Cultivate Gratitude: Intentionally shifting cognitive focus toward present positive aspects of life can significantly enhance resilience and temper feelings associated with grief and loss TTC.
- Truth 8: Practice Intentional Downtime: Actively diminish the background sense of urgency by scheduling and prioritizing periods of genuine relaxation, effectively dismantling the chronic “threat” signaling that powers the Stress and fertility connection mechanism.
Conclusion: Taking Control of the Stress and Fertility Connection Mechanism
The interdependence between psychological strain and reproductive success is nuanced but firmly established. By gaining a precise and meticulous understanding of the underlying biological pathways—from the HPA axis-mediated suppression of hypothalamic hormones to the microscopic injury caused by oxidative stress—we gain the leverage necessary to actively control the Stress and fertility connection mechanism.
While stress is seldom the only etiology for infertility, regulating the Stress and fertility connection mechanism is a fundamental, non-negotiable prerequisite for optimizing general reproductive health and enhancing the efficacy of conception attempts, especially within assisted reproductive technologies (ART).
Compelling clinical evidence affirms that targeted psychological interventions significantly improve outcomes and specifically mitigate the adverse impact of chronic stress on IVF success.
To take meaningful control over the Stress and fertility connection mechanism is to elevate mental well-being to the same priority level as physical health.
By diligently applying these eight essential truths, one moves beyond mere coping to actively cultivating a biologically receptive state of calm that supports the intricate requirements for new life. The genuine capacity to positively affect your fertility journey resides directly in your ability to manage your body’s stress response.
Can stress delay my period?
Undeniably, high psychological or physical stress can induce a delay or even temporary cessation (amenorrhea) of the menstrual period. Acute or chronic stress instructs the hypothalamus—the central orchestrator of the endocrine system—to inhibit the release of Gonadotropin-Releasing Hormone (GnRH). This disruption leads directly to delayed ovulation or stress-induced anovulation, causing a delay in the menstrual flow. This sequence illustrates the direct biological function of the Stress and fertility connection mechanism.
Is male fertility stress as important as female stress?
Yes, male fertility stress warrants equal consideration. Although the mechanism differs, high levels of psychological stress in men can impair endocrine function, leading to decreased testosterone, reduced sperm motility, and elevated levels of sperm DNA damage. Addressing male fertility stress through lifestyle optimization and emotional support is a crucial, integrated component of optimizing the total Stress and fertility connection mechanism for the couple.
What are adrenal fatigue and cortisol, and fertility?
Adrenal fatigue is a term used functionally to describe the systemic exhaustion and nonspecific symptoms (e.g., chronic fatigue, body aches, hyper-vigilance) resulting from chronic HPA axis overstimulation, though it lacks formal medical recognition. The relationship between cortisol and fertility is a key component of the Stress and fertility connection mechanism: excessive, prolonged cortisol production directly suppresses the hypothalamic-pituitary-gonadal (HPG) axis, thereby disrupting the fundamental processes of ovulation and gamete health.
Can chronic stress affect the impact of chronic stress on IVF success?
Absolutely. The impact of chronic stress on IVF success is clinically significant. Sustained stress negatively influences the body’s response to ovarian stimulation, compromises endometrial receptivity, and can impair uterine blood flow, all critical elements for successful implantation. Studies show that patients who engage in systematic stress management before or during their cycles demonstrate improved pregnancy rates, confirming the necessity of controlling the Stress and fertility connection mechanism even within ART.
What are the best stress reduction techniques for TTC?
Effective strategies targeting the Stress and fertility connection mechanism include implementing structured mind-body programs, fertility regimens, specialized Cognitive-Behavioral Therapy (CBT for fertility), regular mindfulness practice, and low-impact movement such as fertility yoga and other structured relaxation exercises. Prioritizing adequate sleep is also foundational, along with proactive engagement with support groups and seeking informed doctor advice on stress and conception for developing resilience.
What is the infertility stress cycle?
The infertility stress cycle describes the circular feedback loop where the intense disappointment and emotional burden of the fertility journey escalates anxiety and stress. This heightened emotional state, manifesting as infertility distress and emotional turbulence, triggers HPA axis overdrive, reinforcing the hormonal imbalance that can cause stress affect conception. Interrupting this negative loop is essential and is best addressed through a structured intervention like a mind-body program for fertility.
Does stress affect egg quality?
Though complex, the Stress and fertility connection mechanism is significantly linked to elevated oxidative stress. Chronic anxiety and trying to conceive (TTC) can raise oxidative stress markers in the ovarian environment, which may, in turn, compromise egg quality over time and reduce viability. Moreover, stress disturbs the critical estrogen-progesterone balance necessary for healthy follicle maturation, thereby indirectly impacting the quality of the ovulated gamete.
How much stress affects fertility?
The most damaging factor is chronic, sustained psychological stress, rather than fleeting, acute episodes. Persistently high levels of the hormone cortisol interfere with the delicate balance of reproductive hormones, leading to cycle irregularities in women and quantifiable reductions in sperm motility and quality in men. Clinically, women exhibiting high levels of the stress biomarker salivary alpha-amylase are statistically less likely to conceive naturally, providing clear, quantifiable evidence of the Stress and fertility connection mechanism.